As more guidance is produced, Nicole Ridgwell explains why the analysis of the detail is vital for GPs to understand exactly what CQC will be prioritising in their assessment and inspections.
As the whole sector will be acutely aware, CQC has now officially rolled out its new Single Assessment Framework for all CQC-regulated providers in England.
In line with this, CQC has started providing more detailed guidance for providers in relation to what these inspections and assessments will look like, and the specifics of the guidance are a must-read for all providers.
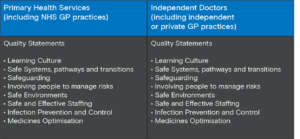
We have known for a while that the new inspection framework has removed the Key Lines of Enquiry (KLOEs) and introduced 34 new Quality Statements and 6 new Evidence Categories, underlined by sector specific evidence and quality indicators:



For providers seeking to understand how to prepare for the new assessments and identify the type of evidence against which assessors will now be judging services the sector-specific evidence and quality indicators are likely to be of most significance.
The Evidence Categories into which this data and information will feed are divided into six general categories:
- People’s experience of health and care services
- Feedback from staff and leaders
- Feedback from partners
- Observation
- Processes
- Outcomes
CQC has advised that evidence from any of these categories may feed into its rating of a service. However, it has also provided details of ‘key evidence categories by sector group’. The guidance confirms that assessors will prioritise collecting evidence in these categories as part of their assessments of any service within that defined sector group. The rationale is that this will allow CQC to tailor the assessment framework to the specific sector relevant to the service being assessed.
It is vital that providers read into and understand the details of what data will be prioritised in their particular assessments. By understanding this, providers will be able to collate data into the categories that CQC will be assessing, in the same way as the KLOEs and Ratings Characteristics previously allowed providers to do. Consequently, this information will also be necessary for any challenges to draft inspection reports (though we note that the format of the new Factual Accuracy Challenge process has changed and that working examples of the new process are only now emerging).
Further analysis of the sector groups themselves, at the least, provokes questions and potentially demonstrates anomalies in the current guidance.
Sector group guidance
There are nine sector groups currently published on CQC’s website, which each have separate guidance with respect to the Evidence Categories relevant to their sector, namely:
- Ambulance services
- Care homes and supported living services
- Community health services and hospices
- Homecare and shared lives services
- Independent doctors
- Independent healthcare single services
- Mental health services
- NHS acute hospital services
- Primary health services
GP Practices appear in two of these: Independent doctors as ‘independent or private GP practices’ and Primary Health Services as ‘NHS GP practices’.
There is a linguistic nuance in the above division, in that all GP Practices are ‘independent’; indeed, they have been since the creation of the NHS in 1948. With the introduction of the 2004 GP contracts, the importance of GPs’ ‘independent contractor status’ was further solidified. This is not, however, simply an interesting linguistic distinction or an excuse to discuss the history of the relationship between GPs and the NHS. It has a potentially fundamental impact on how one GP Practice may be assessed compared to another.
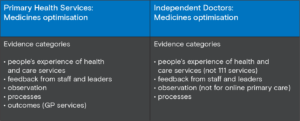
Using the example of the Key Question of Safe, both have the same overarching Quality Statements, however the Evidence Categories that CQC will prioritise in some cases vary significantly. We have used two examples to demonstrate why this is important.
For the Quality Statement of ‘Safe Environments’, for example, CQC will prioritise ‘people’s experience of health and care services’ for ‘independent or private GP practices’ online primary care, but will not do so for ‘NHS GP practices’. This is despite the increased availability of online services through non-private GP Practices since COVID.
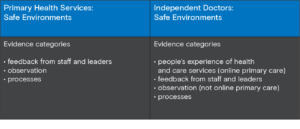
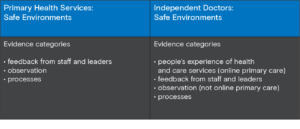
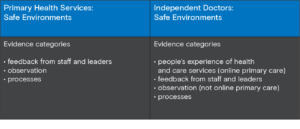
Is it the case that CQC will not be prioritising gathering data on people’s experiences of online care if their GP is not private, or indeed that CQC will not be gathering data on people’s experiences of offline care? That is certainly the implication of the current guidance.
A second example is that of the Quality Statement of ‘Medicines Optimisation’ (whether ‘medicines and treatments are safe and meet people’s needs, capacities and preferences by enabling them to be involved in planning’).
It appears that CQC will prioritise ‘Outcomes’ for ‘NHS GP practices’ but not for ‘independent or private GP practices’.
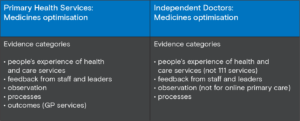
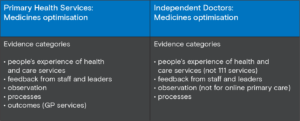
CQC’s own guidance explains that: “Outcomes are focused on the impact of care processes on individuals. They cover how care has affected people’s physical, functional or psychological status”.
And includes measures such as:
- mortality rates
- emergency admissions and re-admission rates to hospital
- infection control rates
- vaccination and prescribing data.
Sourced from:
- patient level data sets
- national clinical audits
- initiatives such as the patient reported outcome measures (PROMs) programme.
Acknowledging the wholesale changes in CQC’s regulatory methods, it’s clear there will be complexities to navigate. The inspection of early adopters likely provided CQC with valuable insights to refine their new approach. Nevertheless, there is concern that some elements of the emerging guidance might conflict with the core principles of this new method. It’s crucial for providers to keep abreast of CQC’s latest guidance, prepare for upcoming inspections within the new framework, and be ready to contest any decisions that seem inconsistent.
How we can help
Our team offers representation and guidance for GP practices facing CQC report challenges, enforcement actions, and issues in employment and commerce. Recognizing the unique nature of each business, we collaborate closely to comprehend your situation and determine the best strategic approach to meet your objectives. Providing comprehensive advice and representation throughout the CQC process, we also support related concerns like safeguarding, inquests, employment, and liaison with commissioners, families, and the media.
Please get in touch with our health and social care lawyers to discuss how we can help at Nicole.Ridgwell@LA-Law.com.

















