This week is Mental Health Awareness Week. We look at the increase in mental health conditions in the last year, treatment options available and where to find the help you may need.
There are multiple types of mental illness including: (1)
- Anxiety disorders (including panic disorder, obsessive-compulsive disorder and phobias)
- Depression, bipolar disorder and other mood disorders
- Eating disorders
- Personality disorders
- Post-traumatic stress disorder
- Psychotic disorders (including schizophrenia).
The statistics show that 1 in 4 adults and 1 in 10 children experience mental illness. (2)
During the 3 lockdowns in the UK, more than half (60%) of adults and over two-thirds of young people (68%) have said that their mental health has got worse during the lockdown. People with pre-existing mental health conditions have likely faced their mental health worsen and people without pre-existing mental health problems have seen their mental health and wellbeing decline. (3)
In 2019, 70 years of the Mental Health Foundation was celebrated. This started in 1949, just after the Second World War. A fund was set up by Derek Richter, a neuro-chemist, who was frustrated at the lack of attention mental health research was getting. By 1989 this had achieved public awareness of mental health problems. This was pivotal and promoted that it was no longer acceptable for mentally ill people to be confined to institutions. Unfortunately, there was still a stigma attached to these kinds of problems.
In 2001, Mental Health Awareness Week was born (then called Mental Health Action Week) and by 2010 we recognised that “a world with good mental health for all is a vision that will take a global movement to achieve”.
Last year in the UK, “kindness” or “be kind” was introduced in Mental Health Week. “The research clearly supports this – it shows that acts of kindness can help improve emotional wellbeing. This is true whether we are giving or receiving it.”(4). Although there is still a stigma, although not as extreme as in the past, this is still widespread.
Mentalhealth.org.uk states that: “In 70 years, we have transformed knowledge of mental health, how it’s caused, treated and prevented. We have helped move services towards the community and away from hospitals and asylums. We have opened the public’s eyes to the need to protect their mental health and prevent problems from occurring and we have set up programmes to help people at all stages of life. Positive steps have been taken towards researching and understanding mental health and there has been a vast improvement in mental health services.”
There is a service that the NHS Community Mental Health Services provide. They work on a structured basis and their framework is a new approach, which offers place-based and integrated mental health support, care and treatment. This enables a more and higher quality of care within the community. This is a core community mental health service that offers care in a residential setting. It contains support from GPs, neighbourhoods and community hubs which makes up the new Primary Care Network. This means that people can access these services through a range of options, in a timely manner from their GP, self-referral online or other digital means. The way it works is shown below:
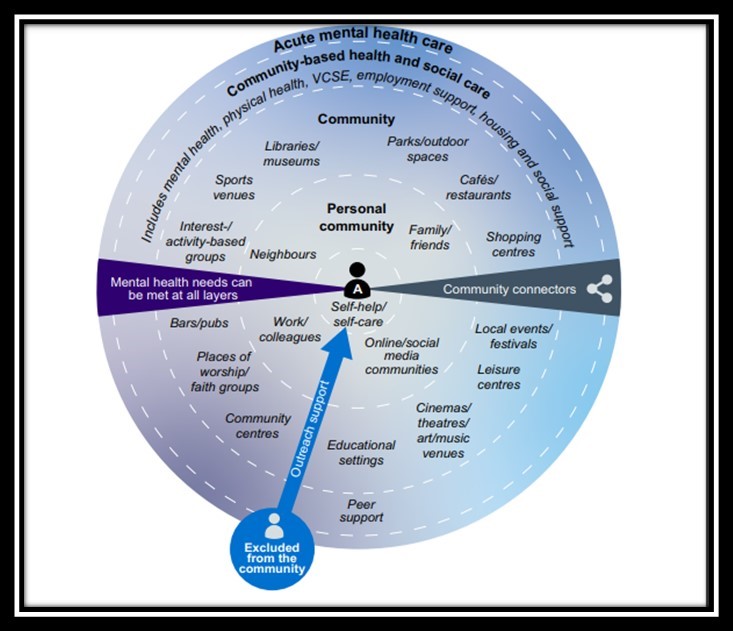
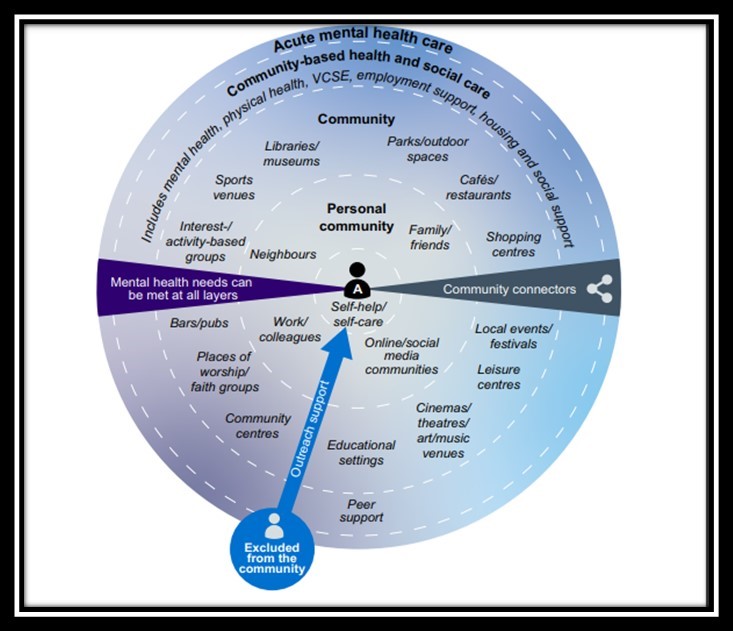
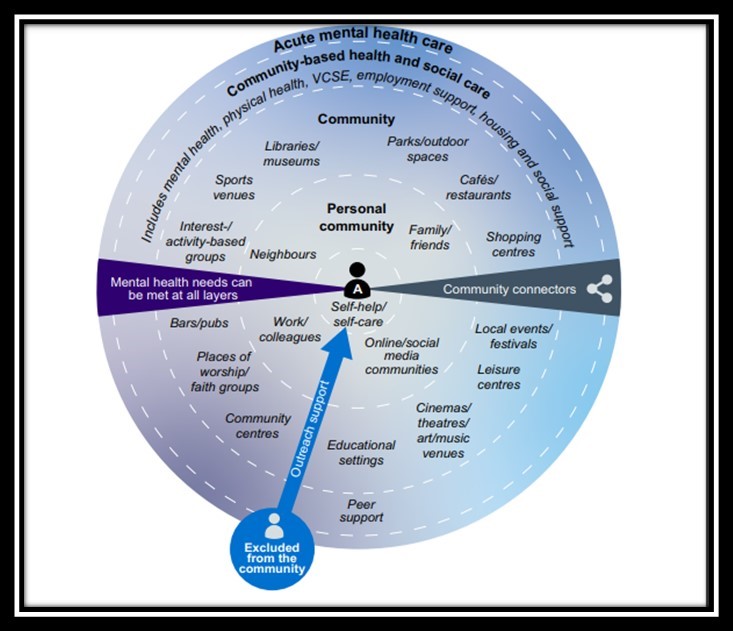
Under this Framework, every person who requires support, care and treatment in the community should have a co-produced and personalised care plan that takes into account all of their needs, as well as their rights under the Care Act, and Section 117 of the Mental Health Act when required.
Over 50% of referrals to CMHTs come from sources other than primary care, including other community or inpatient teams, social care or self-referral. When people’s care moves between teams, typically over 20% of them do not reach the new team. This may be due to complicated referral and transition processes, or a lack of the most appropriate support in one place to address multiple needs. This new framework that has been put in place will stop this from happening as the dedicated Primary Care Network is in place to move patients efficiently from one phase to another.
There are usually long delays between an initial appointment and then patients receiving the care or treatment needed. This approach offers a 4-week waiting time and over the next 2 years will offer cover over 7 regions of England.
Mental health problems are frequently unseen, that is why “be kind” is so important. Little changes in how we all think and what we do can make a huge impact on how the world views mental health. What can you do today to help the cause?
References:
















